The Most Common Causes of Menstrual Irregularities
Aside from being pregnant or going through menopause – which both normally stop a woman from getting her period – here are the other major causes for Menstrual Irregularities (irregular periods or amenorrhea):
- High Stress Levels
When you’re under a lot of stress for an ongoing period, your body can start to conserve energy by preventing ovulation. Experiencing a traumatic event can suddenly cause the adrenals to work overtime, which can disrupt the production of estrogen and other reproductive hormones (a condition called hypothalamic amenorrhea). When you don’t have a lot of estrogen, you aren’t able to properly build up the uterine lining, and as a consequence you don’t get your period.
Why does this happen? Essentially, your body makes sure that emergencies get priority. Comfort is nice and being fertile is important, but it’s still secondary to survival. A built-in survival mechanism that is ingrained in all of us is the ongoing production of crucial “fight or flight” stress hormones like cortisol and adrenaline. Adrenaline and cortisol are the two major players related to our stress responses that help us get away from threats (whether real immediate ones or just perceived ones). Adrenaline and cortisol are completely necessary and sometimes beneficial — helping us to run, climb, exert energy, sweat and regulate our heartbeat, for example — but too much can become a problem.
The body always grants priority to producing these stress hormones that will help you survive a crisis, so sex hormones can take a backseat when your body perceives that “times are tough.” Under chronic stress, there’s not enough raw materials available – such as amino acids that help neurotransmitters to work – to make both sex hormones and stress hormones in some cases, so a choice must be made and the body always chooses stress hormones. Severe stress conditions like dieting, heavy exercise training or intense emotional events are all situations that can induce amenorrhea with or without body weight loss.
- Poor Diet
A poor diet low in nutrients, antioxidants and probiotic food yet high in stimulants can tax the adrenal glands and thyroid. For example, a high intake of sugar, hydrogenated fats and artificial additives, or pesticides is linked with thyroid issues and adrenal fatigue that can raise cortisol.
Excess cortisol hinders the optimal function of many other essential hormones, such as sex hormones. It can also promote the breakdown of bones, skin, muscles and brain tissue when high over a long period of time. This cycle of excess cortisol can lead to protein breakdown, which results in muscle-wasting and potentially osteoporosis.
If you’re struggling with menstruation, make sure to eat enough food and make it the right kind. Eat high antioxidant foods that are nutrient-dense, especially plenty of fats (even saturated fats that are good for you and proteins. Also, choose a high-calorie supplement if you are underweight, have low body fat or are an athlete.
- Extreme Weight Loss and Low Body Weight
When your body mass index (BMI) falls below 18 or 19, you can start to miss your period due to having too little body fat. Body fat is important for creating enough estrogen, which is why very thin women or those with serious conditions like anorexia and bulimia can experience absent or missed periods. Increased physical activity and nutritional demands of intensive exercise can sometimes lead to a low body weight that put you at risk for hormonal problems.
A low-calorie, low-fat diet can also result in nutrient deficiencies and lowered body-fat percentages that may contribute to irregular periods and bone loss. Some reports also show that very lean vegans and vegetarians, including those on fully “raw” diets, might also be at a higher risk – likely because they are more prone to becoming underweight and suffering deficiencies.
- Over-Exercising
Although moderate exercise is very important for ongoing heart health, mood regulation, sleep and maintaining a healthy body weight, too much exercise can also put excess pressure on your adrenal, thyroid and pituitary glands. Women who rapidly start exercising at high intensities — for example, by training for a marathon or some other major event that requires a high level of physical excretion — can stop getting their period suddenly.
Like other stress hormones, cortisol is released in response to any real or perceived stress, which can be physical (including exercise) or emotional. Such stressors include overworking and overtraining, in addition to things like under-sleeping, fasting, infection and emotional upsets. Today, with pressure to stay thin and in shape, some women feel they need to exercise intensely and “break a good sweat” too much and too many days per week.
This kind of exertion can actually increase stress and deplete the body of energy needed to regulate sex hormones. One University of Michigan report found that running and ballet dancing are among the activities most closely associated with amenorrhea. As many as 66 percent of women long-distance runners and ballet dancers experience amenorrhea at one time or another! Shockingly, among women bodybuilders, 81 percent experienced amenorrhea at some point and many had nutritionally deficient diets!
“Exercise-induced amenorrhea” can be an indicator of an overall energy drain and is most common among young women. In fact, female participation in high school athletics has increased 800 percent in the last 30 years, and at the same time hormonal imbalances have also risen. Other concerning issues that sometimes come along with this phenomena include bone density loss and eating disorders. That’s why addressing skeletal problems, heart complications and nutritional deficiencies in this population is a very high priority for physicians.
- Thyroid Disorders
You may never suspect it, but it just might be that your thyroid is the cause of your problems related to hormonal imbalances. Some reports show that thyroid disorders may be one of the leading causes of missed periods, with roughly 15 percent of amenorrhea patients experiencing thyroid irregularities. The thyroid gland, often called a “master gland” and considered a crucial controller of the endocrine system, largely controls your metabolism and impacts many sex hormones.
Thyroid disorders, including hypothyroidism or hyperthyroidism, can cause widespread symptoms like changes in estrogen and cortisol hormones and missed periods. Too much cortisol circulating in the body can lead to overall hormone resistance, including thyroid resistance. This means that the body becomes desensitized to these hormones, and more may be required to do the same job.
- Stopping the Birth Control Pill
Some women stop getting their period somewhat intentionally while on birth control, but even when they stop the pill their period doesn’t return. While some doctors advise that a woman’s period should adjust and return within a few months of stopping the pill, many women experience missed or irregular periods for years afterward.
A woman’s natural menstrual cycle is composed of rising and falling levels of estrogen and progesterone, but taking birth control pills keeps estrogen at a sufficiently high level, which fools the body into thinking it’s pregnant and results in irregular periods. It takes the body many months or even years to correct this and return to homeostasis.
One report published in the American Journal of Obstetrics and Gynecology found that about 29 percent of women experience missed periods for more than three months after going off the pill. My advice: Just say no to birth control pills.
- Ongoing Hormonal Imbalances and Disorders
Polycystic ovarian syndrome (PCOS) is a hormone imbalance in women that negatively impacts ovulation. When a woman has PCOS, she experiences altered levels of sex hormones — including estrogen, progesterone and testosterone — that can result in abnormal body or facial hair growth, weight gain, blood sugar problems, acne, and irregular menstrual cycles. PCOS can be diagnosed by a woman’s gynecologist who will test for hormone levels, review symptoms and family history, and potentially examine the ovaries for cyst growths.
It’s also possible to go through “premature menopause” prior to the age of about 40, which can missed periods, hot flashes, night sweats and vaginal dryness – although this is a less common reason for irregular menstruation.
- Food Allergies and Sensitivities
Undiagnosed gluten sensitivity or celiac disease can both impact hormone levels. Because these conditions can cause nutrient deficiencies, negatively impact gut health and add chronic stress to your adrenal glands, they have the ability to affect sex hormone production.
How to Rebalance Hormones and Bring Back Your Period
As you can see, a woman’s diet, level of stress, relationship with family and friends, habit of exercise, environment, and a host of other factors contribute to the quality of her life and, therefore, her state of hormonal health. While hormone imbalances can often go ignored, it’s crucial for all women to pay honest attention to how each element of their lifestyle affects their health — this way they can make choices to eliminate or tweak any aspects that are causing irregular periods.
If you’ve been missing your period for a while, speak to your doctor about running some important tests. According to a 2010 study, “Evaluation and management of adolescent amenorrhea,” the essential laboratory examinations you should request include follicle-stimulating hormone (FSH), luteinizing hormone (LH), thyroid-stimulating hormone (TSH) and prolactin measurements. Your doctor will also likely completely rule out pregnancy and check for signs of PCOS and early menopause through weight changes, acne, hair growth and other signs related to changes in androgen hormone levels.
Many experts recommend a three-tier treatment strategy for regaining your period and hormonal health:
Make appropriate diet, lifestyle and stress-reduction changes first.
Use natural herbs and remedies when extra support is needed. Only then consider trying hormonal pills or procedures with a healthcare provider, if need be. Lifestyle changes to make include:
- Reduce Stress
Use various lifestyle techniques that are a natural remedy for anxiety in order to combat stress, such as light exercise, healing prayer or meditation, essential oils, journaling, and acupuncture or massage therapy. Few studies have looked at the use of acupuncture for treatment of amenorrhea, but some preliminary trials have found it helpful for women who have widely separated menstrual cycles.
You can also try taking adaptogen herbs, which are a unique class of healing plants that promote hormone balance and protect the body from a wide variety of stress-related diseases. Adapotgens like maca root, ashwagandha and holy basil help with immune function and combat the ill effects of stress. Ashwaganhda can help heal thyroid and adrenal fatigue, for example.
Also, consider if you should also re-evaluate your need for intense competitive exercise, drinking coffee and using other stimulants, pushing yourself too hard at work, under-sleeping, and exposing yourself to toxic or irritant pollutants. Remember that rest and sleep are crucial for hormonal balance, so don’t let an avoidable lack of sleep run you down.
- Improve Your Diet
Eating a variety of nutrient-dense foods is key to keeping your hormones in check. You also want to be sure to have plenty of short, medium and long chain fatty acids that are essential fundamental building blocks for hormones. Some healthy fats to add to your diet include coconut oil, nuts and seeds, avocados, grass-fed butter, and wild-caught fish like salmon.
Probiotics can also help your body produce certain vitamins that affect hormone levels like insulin. Some probiotic foods and supplements to try include: goat’s milk yogurt, bone broth, kefir, kombucha and fermented vegetables.
- Reevaluate Your Exercise Routine
Both too much and too little exercise can be problematic for controlling cortisol and stress hormones. If you experience menstrual problems, trying gentle forms of exercise in moderation might be able to help the problem.
Focus on exercising as a way of reducing stress rather than burning calories to lose weight. Walking, yoga, dancing, light resistance training, and tai chi or qi gong are soft forms of exercise that emphasize and support gentle movement of the body. Doing 30-45 minutes most days can be beneficial, but more than an hour daily, or not giving yourself enough rest, can trigger period problems.
- Steer Clear of Environmental Toxins
You can greatly eliminate toxins in your body by avoiding conventional body care products that are high in hormone-disrupting ingredients like DEA, parabens, propylene glycol and sodium lauryl sulfate. These are all related to altered estrogen production and possibly thyroid and adrenal issues, so check your skin care and household product ingredient labels carefully. Also, try to use glass and stainless steel kitchen equipment and containers instead of plastic or Teflon whenever possible in order to avoid BPAs, hormone disruptors and other chemicals.
Chinese Herbal Treatment for Dysfunctional Uterine Bleeding (DUB)
Menstruation is unique to women. When a woman reaches puberty, her uterus matures and her kidney essence is enriched to a certain extent. The kidneys will then produce a type of substance for promoting sexual functions, which is called Tian Kui (Heavenly water). Under the action of this substance, the conception vessel and thoroughfare vessel meridians are exuberant and flushed with abundant qi and blood. The excessive qi and blood will empty into the uterus and produce regular menses. In old age, the kidney essence is exhausted and Tian Kui declines. The conception vessel and thoroughfare vessel gradually close and become obstructed, a woman then begins to have menstrual irregularities until menopause occurs.
According to traditional Chinese medicine (TCM), menstrual cycles are dominated by rhythmic changes of kidney qi inside the body.
Dysfunctional uterine bleeding (DUB) is characterized by irregular periods, excessive or prolonged menstrual flow, which come under TCM category of “beng-lou“, literally meaning periods come with sudden flooding or trickling for a long time. TCM claims that dysfunctional uterine bleeding can be due to a wide variety of factors, such as an unhealthy lifestyle, poor diet or improper eating habits, lack of exercise, environmental factors, emotional or psychological issues, toxins and hereditary influences. The factors weaken the internal organs, affect blood and qi, and impair the conception vessel and thoroughfare vessel meridians, resulting in an uncontrollable menstrual flow.
TCM physicians usually regard dysfunctional uterine bleeding as a clinical difficulty, since the pathology usually involves several organ systems, as well as qi and blood dysfunctions, which give rise to complex conditions and hard to treat. Early diagnosis and treatment are crucial to prevent it developing into a lingering and worse consequence.
When physicians doing a consultation for dysfunctional uterine bleeding, they will ask about the specific characteristics of the bleeding, including the duration, interval, amount of bleeding, color and texture of the blood, and the accompanying symptoms during the time, other factors like age, medical history and lifestyle also take into account. The remedies are designed according to TCM disharmony patterns, and the therapeutic principles are:
| 1. | Arrest bleeding and regulate the conception vessel and thoroughfare vessel meridians, |
| 2. | Treat the underlying disharmony, such as to invigorate the kidneys and restore their controls over the menstruation, |
| 3. | Restore the inside of the uterus, rebuild a normal menstrual cycle and prevent recurrence. |
 |
 |
 |
||
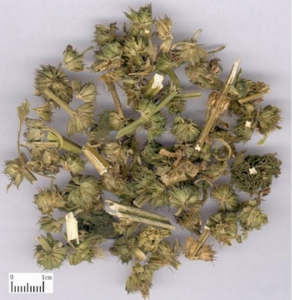
| Argy wormwood leaf | Turmeric root-tuber | Motherwort herb |
Herbal prescriptions for dysfunctional uterine bleeding
For women with dysfunctional uterine bleeding, age, pregnancy and delivery history make particular changes to their bodies, and thus are important considerations for identifying the disharmony patterns. Adolescent girls tend to have kidney deficiency or over-heated blood; women in childbearing age tend to have liver stagnation or over-heated blood; while menopause women tend to have liver and kidney deficiencies or spleen weakness and qi (vital energy) deficiency. The later two age groups often combine with blood stasis too. Below are the common disharmony patterns that involve in dysfunctional uterine bleeding.
Heat in uterus
Sudden heavy vaginal bleeding or persistent vaginal blood dribbling, the blood is red or dark red colored and is thick in texture. Other signs may include mouth dryness, flushed face, dizziness, irritability, scanty urine and dry stool. The tongue is red with yellow coating, and pulse is taut and rapid. The remedy should aim to clear heat, cool blood, consolidate thoroughfare vessel and stop bleeding.
Sample prescription: Modified Clear Heat and Consolidate Menstruation Decoction plus cattail pollen, carbonized hair and motherwort herb
Stasis in uterus
Irregular periods, persistent vaginal blood dribbling, or missed periods follow by a sudden profuse vaginal bleeding, and the blood is dark-purplish and has clots. Other signs may include pain in the lower abdomen that typically feels relieved after passing the blood clots. The tongue is dark-purplish or has purple spots on it, and the pulse is taut or hesitant. The remedy should aim to activate blood, resolve stasis, consolidate thoroughfare vessel and stop bleeding.
Sample prescription: Resolve Stasis and Stop Menorrhagia Decoction plus cattail pollen and India madder rhizome (charred)
Damp-heat in uterus
Irregular periods, persistent vaginal blood dribbling, or sudden profuse vaginal bleeding, the blood is dark red or purplish red in color, thick and sticky in texture. There may also have excessive and foul vaginal discharges, pain and distention in the lower abdomen, thirst, general heaviness, and even fever. The tongue is red and covered by yellow and greasy coating, and the pulse is rolling and rapid. The remedy should aim to clear heat, resolve dampness and stop bleeding.
Sample prescription: modified Three Wonders Sargentglory Vine-stem Decoction
Qi deficiency failing to retain blood
Irregular periods, starts with profuse vaginal bleeding and then becomes persistent vaginal blood dribbling, the blood is light and thin in texture. Other signs include paleness, puffiness, fatigue, breath shortness, poor appetite, loose bowels, and emptiness and heaviness feelings in the lower abdomen, palpitations and general weakness. The tongue is pale, the pulse thready and weak. The remedy should aim to replenish qi and reinforce its ability to astringent blood, invigorate spleen and nourish blood.
Sample prescription: Consolidation and Stop Menorrhagia Decoction plus Chinese yam, bugbane rhizome and India madder rhizome (charred)
Kidney yin deficiency
Irregular periods, excessive vaginal bleeding or persistent vaginal blood dribbling, the blood is bright red color and thick in texture. Other signs include dizziness, ear ringing, warm palms and soles, irritability, lumbar and knee weakness, insomnia and night sweats, red cheeks, fatigue, general weakness and frequent urination. The tongue has little coating, and the pulse is thready and rapid. The remedy should aim to nourish kidney yin, consolidate thoroughfare vessel and stop bleeding.
Sample prescription: Modified Restore the Left (kidney) Pill (delete the achyranthes root in the formula, and add glossy privet fruitand charred garden burnet root)
Kidney yang deficiency
Irregular periods, excessive vaginal bleeding or persistent vaginal blood dribbling, and the blood is light in texture. Other signs include limb coldness, cold pain in the lumbar and knee regions, bright white complexion, profuse urination, and loose bowels. The tongue is pale and bulky, or has teeth marks on the margin, and the pulse is deep and thready in particular for the chi region. The remedy should aim to warm and invigorate kidney yang.
Sample prescription: Modified Restore the Right (kidney) Pill, (delete aconite root and cassia bark in the formula, and add astragalus root, morinda root, and epimdium.
After the bleeding is controlled, intensive treatment should be continuous for three or more cycles. The consolidation therapy is aimed to resume the normal functions of the kidneys, spleen and liver, and rebuild a regular menstrual cycle. Physicians will treat according to age groups, in which adolescent girls need to invigorate the kidneys and smooth the menstrual cycle, childbearing women need to soothe the liver and nourish blood, regulate the menstrual cycle and promote ovulation, menopause women need to invigorate kidneys and spleen and prevent recurrent bleeding. Menopause women should also visit their western doctors and check up regularly to rule out other health problems.
It should be noted that menstrual disturbances can be due to different pathologies and may vary from person to person. The above patterns can appear alone or in mixed form, they are also changeable and may transform into each other over time. There is no exclusive therapy for dysfunctional uterine bleeding, each regime is customized from the independent conditions that exist within each individual; it may also need adjustment during the course of treatment so as to fit the changing condition.

